Does Insurance Reimbursement Impact a Provider’s Clinical Decision Making? Short Answer: ABSOLUTELY!!!
By: David P. Brungo, BSPT, MBA, MS, AIB-VA, AIB-VRII; Expert Contributor: Summerville PT & Balance Rehab for Adults
If you read that Blog Headline and have no idea what it’s really asking, here it is in more simple terms: Most providers, such as your PCP, Neurologist, Orthopedist, Physical Therapist, etc., accept assignment by insurance companies. That means they are contractually obligated to accept ONLY what the insurance decides it will pay for the services provided in addition to the patient’s co-pay and/or deductible. The decisions insurance Boards make about what they will and will not cover, as well as how much they’ll pay to providers for covered services, have a huge impact on a provider’s ability to generate revenues and stay in business competitively. Some providers are “cash based,” which means they do NOT accept what the insurance pays and instead charge the patient directly for all services rendered, after which the patient must submit their claims to their insurance for whatever their insurance would have paid to the provider. We’re going to talk about how a provider’s clinical decision making might be affected by the coverage and reimbursement policies of their patients’ insurance. In other words, how likely is it that a clinician’s real time decisions about what kind of as well as how much care to provide are INFLUENCED BY insurance reimbursement policy? A very common generalized example of this is: Knowing that their patient needs X, Y and Z but the patient’s insurance only provides limited — or perhaps — no coverage/reimbursement at all, for X, Y and Z, will a clinician decide to do something mostly as a function of reimbursement level as opposed to providing what that provider believes their patient ACTUALLY NEEDS and that will be the BEST OVERALL intervention for the patient as opposed to just being the most attractive reimbursement to the provider? Thus, there may be an ethical/professional dilemma to providers that is based entirely on insurance reimbursement policies. The research on this is pretty clear and you may not like what it suggests.
“ETHICS” relating to health care and medicine are culturally defined and shaped by ideological philosophies and values.₁
As a physical therapist, I am required to be guided by professional ethics and standards of conduct just like every other health care provider. Again, these are ideological in nature and may not align very well with reality, including a provider’s need to pay their bills, be “fairly” reimbursed for important and often highly complex health interventions that truly help patients but may not be on “the list” of what’s covered (or perhaps be reimbursed so minimally that a provider may be able to make more by doing something else for their patient that may be clinically necessary or questionably necessary or even not so necessary). But what about the personal motives of individual providers, owners or investors of health care services, such as greed or inability to compete effectively in the local market because other providers can manage this dilemma differently due to their sheer size or their focus on high volume care providing? It’s complicated.
When you look at your Explanation of Benefits (EOB), and you see that the hospital at which you had your total knee replacement surgery charged your insurance well over $100K, realize that they will not be paid that amount because your insurance is never going to pay that amount in the current insurance based provider environment that is constantly complicated by operational budgets and profit motives of human beings (whether as an individual provider, a professional group of physicians or PTs, or a mega-huge research hospital system with very, very deep pockets) as well as the sheer demand for health care services and high cost of health care technology and innovation. All of these forces are in play.
I’ve been in practice for over 30 years. I’ve seen so many changes that have impacted this discussion but they are almost always triggered by insurance based reimbursement policy.
The presence of fraud, waste and abuse in healthcare has been well-established for many years, is a direct reflection of the forces mentioned above, runs directly counter to professional ethics in healthcare and accounts for Billions of dollars of unnecessary expenditures each and every year.₂

I don’t know if you’ve noticed, but our healthcare delivery systems in the USA are becoming more and more consistent with the Big Box store models of operation where BIGGER generally means being better able to compete and, let’s face it, control business revenues and costs. But are there tradeoffs involved, especially to the patient and the care they receive? Most notable among potential tradeoffs to the patient is whether a provider refers you only to a PT Clinic owned by the referring provider or group of investors as opposed to referring the patient to where the patient prefers to go. I can tell you very honestly, we see this on a daily basis and our patients often tell us that they had to fight with the referring provider’s office to actually have their referral redirected to us even though they made it clear to their provider where they preferred to be referred for their PT. While it is not always the case, this general practice by providers might actually be illegal as it relates to the principle of “referral for profit” (aka, “Stark Law”) and has a much different legal applicability for health care providers than it does most other types of professionals and businesses. In South Carolina, the legal rules are very attractive to providers in that it is NOT against the law as the general premise so long as the referral meets pre-defined exceptions.3 While it may NOT be illegal, it may still be quite unethical. This poses a substantial breach of standardized and more fair provider practice guidelines and good luck going through the Legal process of proving unethical referral or practice behaviors by those who fall into the “questionably ethical” group.
While it’s only one piece of this enormously complicated puzzle, insurance reimbursement policies have a significant impact on providers’ practice behaviors4 and play an immense part in this ethical challenge in America, which is often touted as having “the best health care system in the world” anecdotally. The research does not support this claim when compared to other developed countries.5
We can definitely do better than this in America. Our experience as providers has been that most health providers are generally good and honest people who have committed to being excellent providers of high quality care but may not always have the autonomy to make independent decisions about how to treat their patients clinically or to where they are “permitted” to refer them when additional care, such as physical therapy, is needed. Do your homework and choose wisely when contemplating where you’ll go to receive your care and whom you Trust to coordinate that care.

We Can Definitely Do Better Than This in America!!!
1 “Medical Ethics – An Overview of the Basics” (found online at: https://vtethicsnetwork.org/medical-ethics/overview); Vermont Ethics Network, 9/20/2022.
2 “What You Should Know About Health Care Fraud, Waste & Abuse” (found online at: https://www.fighthealthcarefraud.com/); Fight Healthcare Fraud, 9/20/2022.
3 “Fraud and Abuse Laws” (found online at: https://oig.hhs.gov/compliance/physician-education/fraud-abuse-laws/#:~:text=The%20Physician%20Self%2DReferral%20Law%2C%20commonly%20referred%20to%20as%20the,relationship%2C%20unless%20an%20exception%20applies); U.S. Department of Health and Human Services – Office of Inspector General, 9/20/2022.
4 “Discovering Healthcare Provider Behavior Patterns Through the Lens of Medicare Excess Charge” (Sen & Deokar: found online at: https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-020-05876-1); BMC Health Services Research, 9/20/2022.
5 “Mirror, Mirror 2021: Reflecting Poorly – Health Care in the U.S. Compared to Other High-Income Countries” (found online at: https://www.commonwealthfund.org/publications/fund-reports/2021/aug/mirror-mirror-2021-reflecting-poorly); The Commonwealth Fund, 9/20/2022.


 I’m seeing a lot more of my total patients reporting generalized fatigue, lack of energy, weakness, being unsteady on their feet and maybe even a little down in the dumps. Sometimes there are falls involved. There can be many reasons medically as well as pharmaceutically that can contribute to the above symptoms, but it doesn’t take a rocket scientist to realize that these are all 100% explainable as the longer-term effects of having our lives contained during an extended Pandemic. We’re not getting out as much or for as long. We’re likely not socializing nearly as much. Maybe we’re enjoying a little too much sitting time, whether it’s video calling friends, family, teachers, etc., or enjoying a little too much TV entertainment, many of us have been sitting a whole lot more than usual. Our relative increase in inactivity over the past two years will not come rushing back to “normalcy” without some work on your part.
I’m seeing a lot more of my total patients reporting generalized fatigue, lack of energy, weakness, being unsteady on their feet and maybe even a little down in the dumps. Sometimes there are falls involved. There can be many reasons medically as well as pharmaceutically that can contribute to the above symptoms, but it doesn’t take a rocket scientist to realize that these are all 100% explainable as the longer-term effects of having our lives contained during an extended Pandemic. We’re not getting out as much or for as long. We’re likely not socializing nearly as much. Maybe we’re enjoying a little too much sitting time, whether it’s video calling friends, family, teachers, etc., or enjoying a little too much TV entertainment, many of us have been sitting a whole lot more than usual. Our relative increase in inactivity over the past two years will not come rushing back to “normalcy” without some work on your part. The fact is, you don’t want to go after it with uber-intensity as you’ll most likely develop more scar tissue than anything else, which is counter-productive to the development of good physical health in so many ways, such as flexibility and overall muscle function and capacity. Another favorite expression of mine with patients is, “If you wanna PLAY at THIS level, you have to TRAIN at THIS level.” So simple a concept but worth explaining a bit. Think of a marathon runner. That’s someone who can run for over 26 miles. Imagine if someone who has not been engaging in any regular exercise program or progressive running program tried to run a marathon. Maybe their adrenaline and inner drive would get them across the Finish Line, but they’re almost 100% certain to have injured themselves badly with severe damage to their muscles that will cause significant pain and inflammation that could take a few weeks or months and maybe even substantial medical attention to resolve (e.g., see “Rhabdomyolysis”).
The fact is, you don’t want to go after it with uber-intensity as you’ll most likely develop more scar tissue than anything else, which is counter-productive to the development of good physical health in so many ways, such as flexibility and overall muscle function and capacity. Another favorite expression of mine with patients is, “If you wanna PLAY at THIS level, you have to TRAIN at THIS level.” So simple a concept but worth explaining a bit. Think of a marathon runner. That’s someone who can run for over 26 miles. Imagine if someone who has not been engaging in any regular exercise program or progressive running program tried to run a marathon. Maybe their adrenaline and inner drive would get them across the Finish Line, but they’re almost 100% certain to have injured themselves badly with severe damage to their muscles that will cause significant pain and inflammation that could take a few weeks or months and maybe even substantial medical attention to resolve (e.g., see “Rhabdomyolysis”).















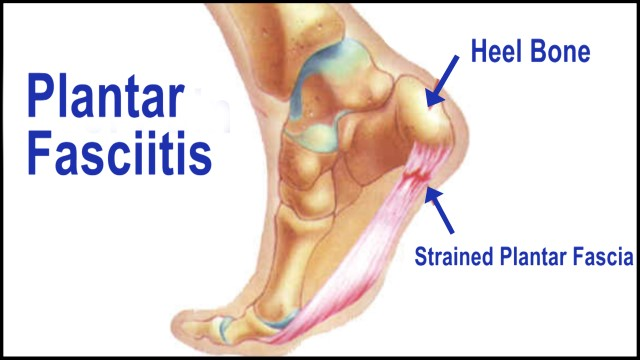

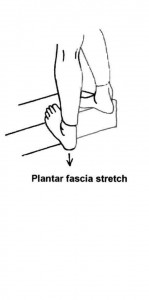
 Should you be bothered by plantar fasciitis, ask your doctor for help and consider physical therapy to effectively and efficiently address the problem. You’ll be back on your feet before you know it!
Should you be bothered by plantar fasciitis, ask your doctor for help and consider physical therapy to effectively and efficiently address the problem. You’ll be back on your feet before you know it!



 By the way, physical therapy doesn’t always have to be “progress oriented” and another recent transformational change affecting physical therapy was a formal clarification during the Obama Administration specifying that PT is appropriate to manage chronic conditions that, in the absence of skilled PT services, would likely cause a progressive decline in functional independence or quality of life. Thus, outpatient PT is very appropriate in cases involving chronic conditions when “progress” may be less likely. Examples of this include weakness on one side of the body remaining after an older stroke or when battling progressive conditions like Ankylosing Spondylitis, Parkinson’s Disease or Multiple Sclerosis.
By the way, physical therapy doesn’t always have to be “progress oriented” and another recent transformational change affecting physical therapy was a formal clarification during the Obama Administration specifying that PT is appropriate to manage chronic conditions that, in the absence of skilled PT services, would likely cause a progressive decline in functional independence or quality of life. Thus, outpatient PT is very appropriate in cases involving chronic conditions when “progress” may be less likely. Examples of this include weakness on one side of the body remaining after an older stroke or when battling progressive conditions like Ankylosing Spondylitis, Parkinson’s Disease or Multiple Sclerosis.

